Revolutionizing Sleep Health: The Role of Artificial Intelligence in Modern Sleep Medicine
The digital age has witnessed artificial intelligence (AI) emerge as a cornerstone of innovation across various industries, with healthcare experiencing some of the most transformative advancements. In sleep medicine, AI fundamentally alters how sleep disorders are diagnosed, treated, and understood, offering promising solutions to some of the most pressing challenges faced by patients and healthcare providers. As technology continues its relentless march forward, AI’s integration into sleep medicine improves clinical outcomes and enhances the efficiency and accuracy of treatments. This paves the way for unprecedented precision in personalized healthcare.
Transforming Diagnosis with AI
Traditional diagnostic methods for sleep disorders, such as obstructive sleep apnea (OSA), often involve cumbersome and expensive polysomnography (PSG) tests. These tests are inconvenient for patients and create bottlenecks within healthcare systems, leading longer to wait times and limited access to diagnostic services. AI, leveraging the power of machine learning (ML) algorithms, promises a revolutionary change in this area. AI can accurately assess sleep quality and identify sleep disorders at their onset by analyzing vast datasets collected from simpler, less intrusive devices like single-lead electrocardiograms (ECGs) and pulse oximeters. This shift not only democratizes access to sleep health services by making them more affordable and convenient but also significantly reduces the logistical burden on medical facilities. This exemplifies how technology is instrumental in streamlining healthcare delivery and expanding its reach (Source).
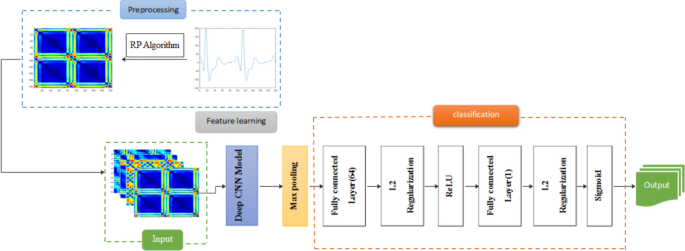
A notable advancement in this field is using convolutional neural networks (CNNs) for analyzing electrophysiological data recorded during sleep. These models excel at processing complex visual data, allowing them to identify patterns in sleep stages and diagnose conditions such as narcolepsy with remarkable accuracy, potentially eliminating the need for extensive manual interpretation by sleep technicians (Source). The potential to automate feature extraction from PSG data is particularly promising, as it can reduce the variability and bias often associated with human scorers, leading to more consistent and objective diagnoses (Source).
Machine learning techniques can uncover new insights from large sleep study datasets, advancing our understanding of sleep’s role in overall health and disease pathways. AI models can identify novel biomarkers, subgroups, and patterns that inform the development of new diagnostic tools and therapies for sleep disorders. For example, the Human Sleep Project (HSP) dataset is being used to develop AI models that provide better-than-human detection of conventional PSG scoring metrics and identify “hidden” information within the brain’s activity during sleep that can be used to directly measure brain health.
Personalizing Sleep Medicine
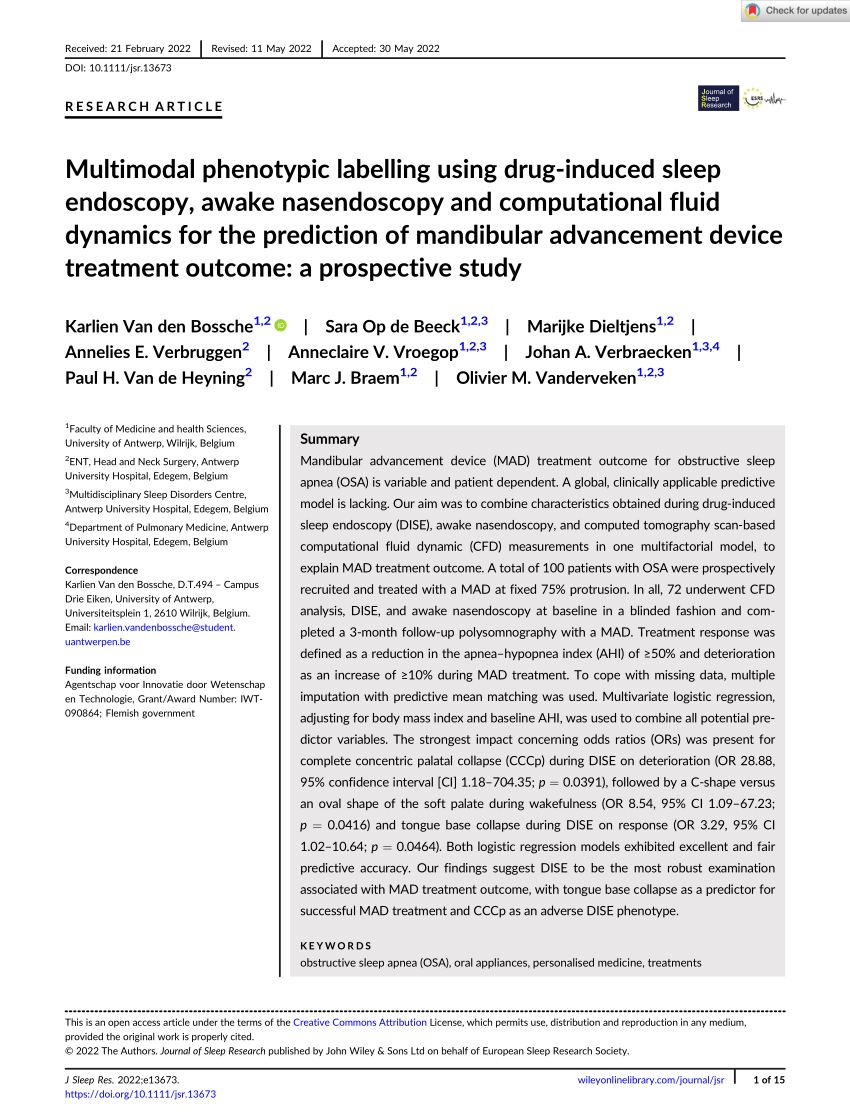
AI’s ability to synthesize and learn from vast amounts of data also opens doors to unprecedented opportunities for personalized medicine. For example, traditional treatment approaches for OSA have focused heavily on the apnea-hypopnea index (AHI), a measure of breathing events during sleep. However, recent advancements incorporate phenotypic approaches that consider the AHI and factors like body mass index (BMI), neck circumference, and even genetic markers (Source). AI algorithms can integrate these diverse data points to tailor treatment plans that are much more effective and individualized for each patient.
Enhancing Pathophysiological Understanding
Beyond diagnostics and treatment, AI is instrumental in enhancing our understanding of the underlying physiological mechanisms of sleep disorders, known as pathophysiology. The integration of computational fluid dynamics with medical imaging, for example, offers valuable insights into the airflow dynamics within the human airway during sleep. Such analyses can help us understand the mechanical properties of the airway in conditions like OSA, where airway collapse during sleep leads to significant disruptions in sleep architecture.

Addressing Challenges and Ethical Considerations
However, the integration of AI into sleep medicine has its challenges. The accuracy and effectiveness of AI systems heavily rely on the quality and diversity of the data used to train them. Biases in training data can lead to skewed AI predictions, which in turn can exacerbate existing health disparities in vulnerable populations. Moreover, using AI in healthcare raises significant privacy and security concerns, particularly when dealing with sensitive health data collected through consumer devices (Source). To mitigate these risks, it is crucial to use diverse, well-curated datasets that reflect the broad spectrum of the population we aim to serve.
It is crucial to ensure that AI tools are validated in clinical settings and that they generalize to a heterogeneous population. Additionally, AI should support but not replace clinicians in the decision-making process, as they are ultimately responsible for patient care.
The Role of Wearable Technology in Sleep Monitoring
The integration of wearable technology into sleep monitoring has brought about significant advancements in how sleep disorders are screened and managed. Devices such as the Apple Watch, Fitbit, and Oura Ring are at the forefront of this revolution, offering a range of features that enable continuous monitoring of sleep patterns and quality. Wearable devices have become increasingly popular for their ability to track various health metrics, including sleep.
Benefits of Wearable Sleep Trackers
1. Continuous Monitoring: Unlike traditional polysomnography (PSG) conducted in sleep labs, wearables provide continuous monitoring over extended periods. This allows for a more accurate representation of an individual’s sleep patterns in their natural environment.
2. Convenience and Accessibility: Wearables are user-friendly and can be worn comfortably throughout the night. They eliminate the need for cumbersome equipment and make sleep monitoring accessible to a broader population.

3. Personalized Insights and Recommendations: Many wearables offer personalized sleep insights and recommendations based on the collected data. This empowers users to make informed decisions about their sleep habits and overall health.
4. Early Detection of Sleep Disorders: By continuously monitoring key health metrics, wearables can help in the early detection of sleep disorders such as sleep apnea. This early intervention can lead to timely treatment and better health outcomes.
Challenges and Considerations
1. Accuracy and Validation: While wearables have shown promise in sleep monitoring, their accuracy compared to PSG is still a topic of ongoing research. Validation studies are necessary to ensure that these devices provide reliable data.
2. Data Privacy and Security: The collection and storage of health data by wearable devices raise concerns about data privacy and security. It is essential to implement robust measures to protect sensitive health information.




















